-
Your Fingers Show Your Athletic Potential and Anxiety
Source:
The Norwegian University of Science and Technology (NTNU)
Summary:
By comparing your index and ring fingers, a neuroscientist can tell if you are likely to be anxious, or if you are likely to be a good athlete.By comparing your index and ring fingers, a neuroscientist can tell if you are likely to be anxious, or if you are likely to be a good athlete.
It is well-known that adults whose index finger is shorter than their ring finger were exposed to greater amounts of testosterone when they were in the womb.
Both women and men with this characteristic are — on average — better equipped to solve mentally demanding 3D rotation tasks as adults. As a group, they also have better physical and athletic abilities, but are more prone to having ADHD and Tourette’s syndrome.
Why on earth is this the case? Both boys and girls are exposed to testosterone in the womb. Everyone has different levels of male and female sex hormones. Some men have a lot of testosterone, some have less, and the same applies to women. Women who have received a lot of prenatal testosterone don’t need much testosterone as adults.
The level of testosterone in utero affects one’s finger length as an adult.
24 women and a drop of testosterone
“The relationship between the index finger and ring finger in particular indicates how much testosterone you have been exposed to in utero,” says Carl Pintzka, a medical doctor and researcher at the National Competence Service for Functional MRI.
In his doctoral dissertation at NTNU, Pintzka investigated how the brain functions differently in women and men. As part of this study, he tested an established theory about the significance of finger length and how the brain works.
He measured the finger length of 42 women and gave half of them a drop of testosterone. The other half were given a placebo. Afterwards, the women had to solve various mental tasks.
Short index finger, more testosterone
“We could then look at how testosterone levels affect different abilities in healthy women both in the womb and in adulthood,” says Pintzka.
An index finger that is relatively short compared to the ring finger indicates that one has been exposed to a lot of testosterone in utero, whereas a relatively long index finger suggests a lower exposure to testosterone in the womb.
“One mechanism behind this relationship is the difference in the receptor density for oestrogen and testosterone in the various fingers in utero. This relationship has also been shown to remain relatively stable after birth, which implies that it’s strictly the fetal hormone balance that determines this ratio,” says Pintzka.
More testosterone, better sense of place
The relationship between the index finger and ring finger in humans is associated with a variety of abilities in adulthood.
“The greatest effect has been found for various physical and athletic measures, where high levels of prenatal testosterone are consistently linked with better capabilities,” Pintzka says. “Beyond this we find a number of uncertain results, but a general feature is that high levels of testosterone generally correlate with superior abilities on tasks that men usually perform better, such as various spatial tasks like directional sense,” he adds.
Conversely, low levels of testosterone are associated with better abilities in verbal memory tasks, such as remembering lists of words. Fetal hormonal balance also likely affects the risk of developing various brain-related diseases.
… but also more ADHD and autism
Pintzka says studies show that high levels of testosterone in utero correlate with an increased risk of developing diseases that are more common in men, such as ADHD, Tourette’s and autism. Low levels of testosterone are associated with an increased risk of developing diseases that are more common in women, like anxiety and depression.
His study primarily involved researching how testosterone affects different spatial abilities in women. The women were asked to navigate a virtual maze, and to mentally rotate different three-dimensional objects.
More study needed According to Pintzka, the study results indicate a trend towards a positive effect of high testosterone levels on spatial abilities in utero. He believes that a larger study would be able to show a significant correlation. Furthermore, the results suggest that these hormone levels are important both in utero and in adulthood.
In other words, no definite conclusions can be drawn quite yet. Pintzka found no prenatal hormonal effects on study participants’ ability to navigate a virtual maze.
“The women who scored best on the mental rotation tasks had high levels of testosterone both prenatally and in their adult lives, while those who scored worst had low levels in both,” says Pintzka.
Journal Reference:
Carl W.S. Pintzka, Hallvard R. Evensmoen, Hanne Lehn, Asta K. Håberg. Changes in spatial cognition and brain activity after a single dose of testosterone in healthy women. Behavioural Brain Research, 2016; 298: 78 DOI: 10.1016/j.bbr.2015.10.056
https://www.sciencedaily.com/releases/2016/10/161012095619.htm
“The Greatest Health of Your Life”℠
Boston Testosterone Partners
National Testosterone Restoration for Men
Wellness & Preventative Medicinehttp://www.BostonTestosterone.com
http://www.facebook.com/bostontestosterone
855-617-MEDS (6337) -
Progesterone: A Key Ingredient for Optimal Health
There seems to be a common misconception among physicians and patients that all hormones are the same. Of course, this is not true, but it shows the pharmaceutical propaganda machine is working. The basic difference between chemical hormones and natural hormones is that one has side-effects and the other does not. This is because side-effects are a property of drugs not foods. Consequently, it follows that hormones obtained from natural food sources, also known as “bio-identical hormones,” do not have the same negative effects associated with synthetic hormone drug products.
The most common prescription hormone drugs include various forms of estrogen and progestin, a synthetic progesterone that acts more like estrogen than progesterone. Female patients are typically prescribed these synthetic hormone drugs to help with their menstrual cycle or menopause. In general, estrogen has a very broad physiological role for males as well as females. The effects of estrogen include, but are not limited to, the following: water retention, aging, stress, memory loss, hypoglycemia, increased fat, hypothyroidism, miscarriage, infertility, uterine fibroids, blood clotting, vascular spasm, increased cholesterol, gall bladder disease, and cancer.
The main cause of hormone-related health problems in women is not due to the absolute deficiency of estrogen or progesterone but rather the relative dominance of estrogen and relative deficiency of progesterone. For this reason, hormone replacement therapy (HRT) with estrogen alone without an opposing progesterone, such as the prescription drug Premarin, should be avoided. This chemicalized hormonal substitute differs from the natural estrogen in one’s body and contributes to increased estrogen. Increased estrogen, in turn, increases the risk of DNA damage, cancer (e.g., endometrial, breast cancer, etc.), and estrogen dominance. Other contributing factors to excess estrogen include adrenal fatigue, environmental estrogen, obesity, stress, poor diet, and lack of exercise.
Estrogen excess may result in such common maladies as depression, weight gain insomnia, anxiety, blood sugar imbalance, migraine headaches, and chronic fatigue due to adrenal gland exhaustion. Moreover, stress can result not only in adrenal gland exhaustion, but reduced progesterone output and increased estrogen production. A further reduction in progesterone output contributes to all the problems associated estrogen dominance (“Acute stress persistently enhances estrogen levels in the female rat,” Shors et al., Stress. 3(2):163-71, 1999
Interestingly, nature has provided us with progesterone, which acts as an antagonist to estrogen. For example, estrogen stimulates breast cysts while progesterone protects against breast cysts. Estrogen enhances salt and water retention while progesterone is a natural diuretic. Estrogen is associated with breast and endometrial cancers, while progesterone has a cancer preventive effect. In fact, studies have shown that premenopausal women deficient in progesterone had 5.4 times the risk of breast cancer compared to healthy women (“Breast cancer incidence in women with a history of progesterone deficiency,” Cowan et al., Am J Epidemiol, 114(2):209-17, Aug 1981).
Here are some answers to frequently asked questions that patients have about progesterone:
1. Is progesterone supplementation safe? Yes. No side effects have been attributed to natural progesterone in either the scientific or medical literature. While large doses of estrogen have been found to destroy certain areas of the adrenal cortex, large doses of progesterone have been shown to have anti-stress effects without harming the adrenals.
2. Should I take progesterone if I’m pregnant? A “Medical News” item in a 1976 issue of JAMA reports a study showing that progesterone probably plays a critical role in preventing rejection of the fetus by the mother. Its use before and during pregnancy is also associated with a reduced incidence of birth defects. Studies in animals have also shown that prenatal progesterone increases brain size, which is associated with a long life. Conversely, excess estrogen reduces brain size and damages behavior, which may, in turn, adversely affect a subsequent generation (“The Epigenetics of Sex Differences in the Brain,” McCarthy et al.J Neurosci. 2009 Oct 14; 29(41):12815–12823).
3. Can I use progesterone for weight loss? Yes. The primary reasons for using progesterone for weight loss purposes are to decrease the effects of insulin and adrenaline. This is because insulin transports sugar into the fat tissue for storage which, in turn, stimulates the release of adrenaline to raise sugar levels again creating a positive feedback loop. Consequently, as the episodes of hypoglycemia decrease the production of adrenaline to counteract hypoglycemia also decreases. Decreased adrenaline means that less sugar is produced, less insulin is needed for storing sugar as fat, and thus, more weight can be lost.
4. Does progesterone help with insomnia? Yes. Progesterone, which is most highly concentrated in the brain tissue, increases GABA production in the brain which, in turn, promotes sleep.
5. What is the recommended daily dosage of progesterone? The physiologic dose of progesterone for the non- pregnant female is 10-50 mg/day and 10 mg/day in the post-menopausal female. Pregnenolone, a precursor to progesterone, may be taken as anywhere from 30-150 mg/day for women whereas the physiologic of pregnenolone for a man is 5-10 mg/day. In general, the best time to use progesterone for weight loss is 1-3 minutes before eating.
by Daniel F. Royal, DO, HMD, JD Owner of the Royal Medical Clinic, Henderson, NV
“The Greatest Health of Your Life”℠
Boston Testosterone Partners
National Testosterone Restoration for Men
Wellness & Preventative Medicinehttp://www.BostonTestosterone.com
http://www.facebook.com/bostontestosterone
855-617-MEDS (6337) -
DHEA and Pregnenolone
Our review of the scientific literature decades ago indicated that when used appropriately, these bioidentical hormones may slow the onset of multiple degenerative diseases and sustain optimal cognitive function in maturing individuals. Since then, an armada of published studies has validated our position. Just last year, there were 380 newly published papers about DHEA.1
This wealth of incontrovertible medical evidence has not stopped the government from erecting regulatory barriers that would deny you the ability to replenish DHEA and pregnenolone to youthful levels.
The latest governmental assault comes out of California. The sale of DHEA and pregnenolone is now illegal unless accompanied by a fear-mongering, scientifically baseless warning label.
We think the State of California should have consulted enlightened, reputable scientists before imposing such onerous statutory burdens. In this instance, this legislative mandate only serves to misinform and frighten the public about the health-promoting properties of hormones made by our own bodies.
Once again, it is time to set the record straight regarding the medically established benefits of DHEA and pregnenolone.
The infinite wisdom of elected lawmakers in California has spawned a questionable dictate. While few if any of these legislators have any direct experience with DHEA or pregnenolone, they nonetheless have issued a decree that all labels must carry a warning. The warning is so strong that novices who read these labels will fear DHEA and pregnenolone and not use them. That’s too bad since hard science substantiates both the safety and efficacy of these natural hormones.
Life Extension’s medical experts reviewed California’s label information, and our assessment of the peer-reviewed literature differs in certain important respects from the conclusions reached by State legislators.
The law, Section 110423(b) of the California Health and Safety Code, states, “The sale or distribution of dietary supplements containing steroid hormone precursors is prohibited unless the product label for the dietary supplements clearly, and conspicuously contains the following warning:
WARNING: NOT FOR USE BY INDIVIDUALS UNDER THE AGE OF 18 YEARS. DO NOT USE IF PREGNANT OR NURSING. Consult a physician or licensed qualified healthcare professional before using this product if you have, or have a family history of, breast cancer, prostate cancer, prostate enlargement, heart disease, low “good” cholesterol (HDL), or if you are using any other dietary supplement, prescription drug, or over-the-counter drug. Do not exceed recommended serving. Exceeding recommended serving may cause serious adverse health effects. Possible side effects include acne, hair loss, hair growth on the face (in women), aggressiveness, irritability, and increased levels of estrogen. Discontinue use and call a physician or licensed qualified healthcare professional immediately if you experience rapid heartbeat, dizziness, blurred vision, or other similar symptoms. KEEP OUT OF REACH OF CHILDREN.
Separate cautions for pregnenolone must now include the statements that: “Pregnenolone may affect levels of other hormones, such as progesterone, estrogen, testosterone, and/or DHEA. Do not take this product if you have a history of seizures. Do not take this product if you have breast cancer, prostate cancer, or other hormone-sensitive diseases.” And the caution for DHEA now must read, “Do not use DHEA if you are at risk for or have been diagnosed as having any type of hormonal cancer, such as prostate or breast cancer.”
The published literature on DHEA and pregnenolone as supplements paints a rather different picture.
Supplementation with DHEA and/or Pregnenolone—The Scientific Truth
Cancer Risk
The truth, as always, is more nuanced. Important work by Harvard urologist Abraham Morgentaler and others has revealed that low testosterone levels increase prostate cancer risk.2,3 Morgentaler himself has become a strong proponent of supplementation with testosterone in older men.3 He was also the lead researcher on a study demonstrating that DHEA supplementation in rats enhanced total testosterone levels without producing any deleterious changes in prostate tissue.4Both pregnenolone and DHEA are “parent” hormones of the sex hormones estrogen, progesterone, and testosterone. Taking pregnenolone or DHEA supplements, therefore, may indeed raise levels of those sex hormones; in fact, that is considered one of the desired effects. Mainstream physicians, however, continue to express concern about boosting sex hormone levels late in life, citing the theoretical risk of hormone-dependent malignancies such as breast and prostate cancers.
Similar theoretical risks apply for breast cancer. But no increased risk of breast cancer has been demonstrated in large studies of combinations of natural estradiol and progesterone (the natural products of DHEA and/or pregnenolone).5 Furthermore, natural progesterone alone may reduce cancer risk, again suggesting that boosting sex hormone levels with precursors such as DHEA and pregnenolone is safe.6 One recent animal study demonstrates a direct anti-cancer effect of DHEA in obese rats.7
To date, no study has convincingly shown an increase in human hormone-dependent cancer risk as a result of DHEA or pregnenolone supplementation.8 Naturally, any individual who is known to have cancer of any kind should consult with his/her physician when using any new supplement or medication.
Heart Disease or Low HDL
One of the most perplexing features of the California label requirement is the caution about a family history of heart disease or low high-density lipoprotein (HDL) cholesterol.
DHEA is in fact known to decrease cardiovascular risk factors by improving vascular remodeling in the face of high blood pressure, improving insulin sensitivity and reducing obesity, and increasing HDL levels. 9-12 No studies have been published demonstrating that pregnenolone raises any cardiovascular risk factors.
WHAT YOU NEED TO KNOW: ERRONEOUS REGULATION OF DHEA AND PREGNENOLONE
- A California law requires strict labeling for two commonly used supplements, DHEA and pregnenolone.
- Both have a longstanding track record of delaying or reversing multiple diseases of aging and cognitive impairment.
- Both also have impeccable safety profiles, as attested by the experience of millions of users over more than a decade.
- The label requirements reflect a concern about the theoretical risk of hormone-dependent cancers, despite a complete lack of peer-reviewed scientific evidence supporting this claim.
- Other risks mentioned in the label do not even have a sensible theoretical basis, such as those for cardiovascular disease, visual disturbances, or vertigo.
- As with all supplements and medications, prudence suggests careful monitoring of one’s state of health, discussion of any new symptoms with a healthcare provider, and discontinuation of any treatment that produces unwelcome effects.
Rapid Heartbeat, Dizziness, or Blurred Vision
There are no published, peer-reviewed articles suggesting that either DHEA or pregnenolone supplements are associated with rapid heartbeat, tachycardia, or atrial or ventricular fibrillation. In fact, men with atrial fibrillation were shown in one study to have abnormally low DHEA levels.13The California label requirement explicitly warns against continuing supplementation in the face of rapid heartbeat, dizziness, blurred vision, or other “similar symptoms.” This, like the general cardiovascular precaution, is mystifying in the face of the published literature.
Similarly, there is no published report of either DHEA or pregnenolone in association with any visual disturbance or glaucoma. Just two reports exist on age-related macular degeneration and DHEA levels. The older one suggests that higher DHEA levels might be associated with increased risk, but the more recent article demonstrates a protective effect of higher DHEA levels.14,15 And a single French study demonstrated that higher DHEA levels are associated with reduced risk of cataracts.16
Just one study, from 1998, shows in an animal study that pregnenolone produces an excitatory effect on nerve cells in the inner ear, where balance is maintained.17 This could produce a theoretical risk of dizziness or vertigo, but no report of such an effect in humans has been published.
WHAT IS DHEA?
Dehydroepiandrosterone (DHEA) is the most common adrenal steroid hormone in the body.25 It is naturally produced from cholesterol (as are all steroid hormones) in a variety of tissues, most notably the adrenal glands. DHEA is the “parent” hormone of both the androgens and the estrogens (male and female hormones, respectively).26Like the sex hormones themselves, natural levels of DHEA decline with advancing age. That decline creates an increased vulnerability to chronic illnesses such as the metabolic syndrome, osteoporosis, and cardiovascular disease.25 Low DHEA levels are also strongly associated with susceptibility to falls and fractures, and even with earlier death in men.27,28 DHEA has long been used as a natural supplement to restore blood levels to those found in younger adults. Levels of sex hormones rise beneficially during supplementation, while levels of stress-related cortisol drop.29,30 As a result, we typically see improvements in muscle strength and bone mineral density, with a reduction in body fat mass.31,32 Indeed, there is now substantial support for DHEA supplementation in adrenal insufficiency, hypopituitarism, osteoporosis, systemic lupus, depression and schizophrenia.33Importantly, DHEA supplementation in women aged 70-79 also improved sexual desire, arousal, activity, and satisfaction, while also improving menopausal symptoms in younger women.34,35
Perhaps the most impressive benefits of DHEA supplementation are in the realm of cognitive function. Both DHEA and pregnenolone are so-called “neurosteroids,” which protect brain cells from damage by both acute injury and chronic stimuli.36-38 Daily supplements of 25 mg DHEA can increase cognitive scores and prevent deterioration of scores for activities of daily living.39 And many studies have verified the importance of DHEA supplements for improving clarity of thinking and a general sense of well-being.25,26,37
Virilization
Because both DHEA and pregnenolone boost natural levels of testosterone as well as estrogen, there is some concern that women who take the supplements might express more masculine traits such as male pattern baldness, hair growth on the face, and aggressive behaviors. In practice, however, these effects appear infrequently and are mild and reversible when they do occur.18,19
A sensible recommendation for anyone taking DHEA or pregnenolone is to monitor oneself for any of these mild side effects, and to discontinue use or reduce dose if those effects outweigh the benefits of continued supplementation.
Seizure History
WHAT IS PREGNENOLONE?
Like DHEA, pregnenolone is a naturally produced steroid hormone that acts as a “parent” to a variety of other hormones, including the sex steroids and hormones vital for controlling blood mineral content and metabolism. Pregnenolone is also a potent neurosteroid, protecting brain cells from age-related damage and preserving their function.36 In fact, pregnenolone is being explored for use in acute management of brain injury and stroke.40,41 Normal brain tissue contains large amounts of pregnenolone, and animal studies reveal that the steroid enhances development of new brain cells.42,43 In humans, pregnenolone supplementation produces significant improvements in both depression and schizophrenia.44-47 And pregnenolone shows promise in mitigating memory loss and even some of the abnormal structural findings in Alzheimer’s disease.48-50
Pregnenolone also has calming, anti-stress effects in humans, attributed to its ability to modulate brain receptors for certain neurotransmitters. Remarkably, when used in conjunction with the common anti-anxiety drug diazepam (Valium®), pregnenolone reduced the sedative side effects without affecting the anti-anxiety effects.51
Summary
California’s warning label requirement significantly overstates any risks associated with DHEA and pregnenolone as supplements. Despite the dire wording on the required label, there remains no convincing evidence that either supplement, taken at recommended doses, increases cancer risks in humans.
The other risks mentioned in the required warning label either occur rarely or are reversible (hair growth), occur in well-defined populations who should avoid using the supplements (seizure patients), or have no credible basis in the peer-reviewed literature (cardiovascular risk, lipid disturbances, vision disturbances, dizziness).
On the other hand, millions of people worldwide have been using both supplements for more than two decades, during which time no serious adverse events have ever been reported in the world literature or in the FDA’s intense adverse event monitoring system.11
Readers should understand that the cautions on labels of DHEA and pregnenolone supplements reflect an “abundance of caution” on the part of the California rule-makers…or perhaps the wishes of pharmaceutical lobbyists who fear too many people are protecting themselves against age-related disease by maintaining youthful hormone balances.
The overwhelming evidence in the global, peer-reviewed literature suggests exactly the opposite, namely that these supplements are safe and effective when used as directed by health-conscious adults.
If you have any questions on the scientific content of this article, please call a Life Extension® Health Advisor at 1-866-864-3027.
WHAT GERMANY KNOWS THAT CALIFORNIA DOESN’T
Here is an example of a published abstract of a study on DHEA from a German scientific journal. Apparently, the authors at the Department Trauma Surgery, University Hospital of Essen in Germany know something that the California authorities don’t know. First of all, the study states that “DHEA…is free of major side effects….” Secondly, they point out that DHEA may be a significant therapy for trauma and that “several data demonstrate the beneficial effect of DHEA in situations of critical illness including trauma hemorrhage and sepsis. Accordingly DHEA improved the survival rate and clinical situation in several animal models of trauma hemorrhage and systemic inflammation.”
Dehydroepiandrosterone (DHEA): a steroid with multiple effects. Is there any possible option in the treatment of critical illness?52
Curr Med Chem. 2010;17(11):1039-47.
Oberbeck R, Kobbe P.
Department Trauma Surgery, University Hospital of Essen, Hufeland Str. 55, 45141 Essen, Germany. reineroberbeck@hotmail.com
Abstract
DHEA is the major circulating steroid in human blood and it is a central intermediate in the metabolic pathway of sex steroid hormone formation. Although the specific effect of DHEA is still unclear it was demonstrated that DHEA modulates several physiologic processes including metabolism and cardiovascular function. Furthermore, a profound immunomodulatory effect of DHEA was reported. Several data demonstrate the beneficial effect of DHEA in situations of critical illness including trauma hemorrhage and sepsis. Accordingly DHEA improved the survival rate and clinical situation in several animal models of trauma hemorrhage and systemic inflammation. This effect was paralleled by profound changes of immunologic parameters, organ function, and heat shock protein production. Therefore, it was claimed that DHEA may be a new alternative/additive in the treatment of trauma and sepsis. In line, DHEA is a frequently used drug in the field of anti-aging medicine, it is an over-the-counter drug in several countries, and it was reported that DHEA medication is free of major side effects. Therefore, DHEA could easily be used in a clinical trial investigating its effects in critical ill patients. This article reviews the reported effects of DHEA on the base of the literature with the specific focus on trauma and sepsis/critical illness including its clinical perspectives.
The above abstract is copyrighted and reprinted with permission from Bentham Science Publishers, Ltd.
References 1. Available at: http://www.ncbi.nlm.nih.gov/pubmed?term=dehydroepiandrosterone%20 . Accessed April 28, 2011. 2. Morgentaler A. Turning conventional wisdom upside-down: Low serum testosterone and high-risk prostate cancer. Cancer. 2011 Mar 1.
3. Morgentaler A, Lipshultz LI, Bennett R, Sweeney M, Avila D Jr., Khera M. Testosterone therapy in men with untreated prostate cancer. J Urol. 2011 Feb 18.
4. Rhoden EL, Gobbi D, Rhoden CR, et al. Effects of chronic administration of dehydroepiandrosterone on serum testosterone levels and prostatic tissue in rats. J Urol. 2003 Nov;170(5):2101-3.
5. Mueck AO, Seeger H, Buhling KJ. Use of dydrogesterone in hormone replacement therapy. Maturitas. 2009 Dec;65 Suppl 1:S51-60.
6. Seeger H, Mueck AO. Are the progestins responsible for breast cancer risk during hormone therapy in the postmenopause? Experimental vs. clinical data. J Steroid Biochem Mol Biol. 2008 Mar;109(1-2):11-5.
7. Hakkak R, Shaaf S, Jo CH, MacLeod S, Korourian S. Dehydroepiandrosterone intake protects against 7,12-dimethylbenz(a)anthracene-induced mammary tumor development in the obese Zucker rat model. Oncol Rep. 2010 Aug;24(2):357-62.
8. Krysiak R, Frysz-Naglak D, Okopień B. Current views on the role of dehydroepiandrosterone in physiology, pathology and therapy. Pol Merkur Lekarski. 2008 Jan;24(139):66-71.
9. Dumas de la Roque E, Savineau JP, Bonnet S. Dehydroepiandrosterone: A new treatment for vascular remodeling diseases including pulmonary arterial hypertension. Pharmacol Ther. 2010 May;126(2):186-99.
10. Haffner SM, Valdez RA. Endogenous sex hormones: impact on lipids, lipoproteins, and insulin. Am J Med. 1995 Jan 16;98(1A):40S-47S.
11. Labrie F. DHEA, important source of sex steroids in men and even more in women. Prog Brain Res. 2010;182:97-148.
12. Sanchez J, Perez-Heredia F, Priego T, et al. Dehydroepiandrosterone prevents age-associated alterations, increasing insulin sensitivity. J Nutr Biochem. 2008 Dec;19(12):809-18.
13. Ravaglia G, Forti P, Maioli F, et al. Dehydroepiandrosterone-sulfate serum levels and common age-related diseases: results from a cross-sectional Italian study of a general elderly population. Exp Gerontol. 2002 May;37(5):701-12.
14. Defay R, Pinchinat S, Lumbroso S, Sutan C, Delcourt C. Sex steroids and age-related macular degeneration in older French women: the POLA study. Ann Epidemiol. 2004 Mar;14(3):202-8.
15. Tamer C, Oksuz H, Sogut S. Serum dehydroepiandrosterone sulphate level in age-related macular degeneration. Am J Ophthalmol. 2007 Feb;143(2):212-16.
16. Defay R, Pinchinat S, Lumbroso S, Sultan C, Papoz L, Delcourt C. Relationships between hormonal status and cataract in french postmenopausal women: the POLA study. Ann Epidemiol. 2003 Oct;13(9):638-44.
17. Yamamoto T, Yamanaka T, Miyahara H, Matsunaga T. The neurosteroid pregnenolone sulfate excites medial vestibular nucleus neurons. Acta Otolaryngol Suppl. 1998;533:22-5.
18. Rommler A. Adrenopause and dehydroepiandrosterone: pharmacological therapy versus replacement therapy. Gynakol Geburtshilfliche Rundsch. 2003 Apr;43(2):79-90.
19. van Vollenhoven RF. Dehydroepiandrosterone for the treatment of systemic lupus erythematosus. Expert Opin Pharmacother. 2002 Jan;3(1):23-31.
20. Reddy DS. Neurosteroids: endogenous role in the human brain and therapeutic potentials. Prog Brain Res. 2010;186:113-37.
21. Reddy DS, Kulkarni SK. Proconvulsant effects of neurosteroids pregnenolone sulfate and dehydroepiandrosterone sulfate in mice. Eur J Pharmacol. 1998 Mar 12;345(1):55-9.
22. Kokate TG, Juhng KN, Kirkby RD, Llamas J, Yamaguchi S, Rogawski MA. Convulsant actions of the neurosteroid pregnenolone sulfate in mice. Brain Res. 1999 Jun 12;831(1-2):119-24.
23. Maciejak P, Czlonkowska AI, Bidzinski A, et al. Pregnenolone sulfate potentiates the effects of NMDA on hippocampal alanine and dopamine. Pharmacol Biochem Behav. 2004 Aug;78(4):781-6.
24. Williamson J, Mtchedlishvili Z, Kapur J. Characterization of the convulsant action of pregnenolone sulfate. Neuropharmacology. 2004 May;46(6):856-64.
25. Perrini S, Laviola L, Natalicchio A, Giorgino F. Associated hormonal declines in aging: DHEAS. J Endocrinol Invest. 2005;28(3 Suppl):85-93.
26. Johnson MD, Bebb RA, Sirrs SM. Uses of DHEA in aging and other disease states. Ageing Res Rev. 2002 Feb;1(1):29-41.
27. Bischoff-Ferrari HA, Orav EJ, Dawson-Hughes B. Additive benefit of higher testosterone levels and vitamin D plus calcium supplementation in regard to fall risk reduction among older men and women. Osteoporos Int. 2008 Sep;19(9):1307-14.
28. Enomoto M, Adachi H, Fukami A, et al. Serum dehydroepiandrosterone sulfate levels predict longevity in men: 27-year follow-up study in a community-based cohort (Tanushimaru study). J Am Geriatr Soc. 2008 Jun;56(6):994-8.
29. Genazzani AR, Pluchino N, Begliuomini S, et al. Long-term low-dose oral administration of dehydroepiandrosterone modulates adrenal response to adrenocorticotropic hormone in early and late postmenopausal women. Gynecol Endocrinol. 2006 Nov;22(11):627-35.
30. Forsblad-d’Elia H, Carlsten H, Labrie F, Konttinen YT, Ohlsson C. Low serum levels of sex steroids are associated with disease characteristics in primary Sjogren’s syndrome; supplementation with dehydroepiandrosterone restores the concentrations. J Clin Endocrinol Metab. 2009 Jun;94(6):2044-51.
31. Weiss EP, Shah K, Fontana L, Lambert CP, Holloszy JO, Villareal DT. Dehydroepiandrosterone replacement therapy in older adults: 1- and 2-y effects on bone. Am J Clin Nutr. 2009 May;89(5):1459-67.
32. Kenny AM, Boxer RS, Kleppinger A, Brindisi J, Feinn R, Burleson JA. Dehydroepiandrosterone combined with exercise improves muscle strength and physical function in frail older women. J Am Geriatr Soc. 2010 Sep;58(9):1707-14.
33. Binello E, Gordon CM. Clinical uses and misuses of dehydroepiandrosterone. Curr Opin Pharmacol. 2003 Dec;3(6):635-41.
34. Buvat J. Androgen therapy with dehydroepiandrosterone. World J Urol. 2003 Nov;21(5):346-55.
35. Stomati M, Monteleone P, Casarosa E, et al. Six-month oral dehydroepiandrosterone supplementation in early and late postmenopause. Gynecol Endocrinol. 2000 Oct;14(5):342-63.
36. Leskiewicz M, Jantas D, Budziszewska B, Lason W. Excitatory neurosteroids attenuate apoptotic and excitotoxic cell death in primary cortical neurons. J Physiol Pharmacol. 2008 Sep;59(3):457-75.
37. Schlienger JL, Perrin AE, Goichot B. DHEA: an unknown star. Rev Med Interne. 2002 May;23(5):436-46.
38. Roglio I, Bianchi R, Gotti S, et al. Neuroprotective effects of dihydroprogesterone and progesterone in an experimental model of nerve crush injury. Neuroscience. 2008 Aug 26;155(3):673-85.
39. Yamada S, Akishita M, Fukai S, et al. Effects of dehydroepiandrosterone supplementation on cognitive function and activities of daily living in older women with mild to moderate cognitive impairment. Geriatr Gerontol Int. 2010 Oct;10(4):280-7.
40. Shirakawa H, Katsuki H, Kume T, Kaneko S, Akaike A. Pregnenolone sulphate attenuates AMPA cytotoxicity on rat cortical neurons. Eur J Neurosci. 2005 May;21(9):2329-35.
41. Wojtal K, Trojnar MK, Czuczwar SJ. Endogenous neuroprotective factors: neurosteroids. Pharmacol Rep. 2006 May-Jun;58(3):335-40.
42. Jo DH, Abdallah MA, Young J, Baulieu EE, Robel P. Pregnenolone, dehydroepiandrosterone, and their sulfate and fatty acid esters in the rat brain. Steroids. 1989 Sep;54(3):287-97.
43. Mayo W, Lemaire V, Malaterre J, et al. Pregnenolone sulfate enhances neurogenesis and PSA-NCAM in young and aged hippocampus. Neurobiol Aging. 2005 Jan;26(1):103-14.
44. Marx CE, Keefe RS, Buchanan RW, et al. Proof-of-concept trial with the neurosteroid pregnenolone targeting cognitive and negative symptoms in schizophrenia. Neuropsychopharmacology. 2009 Jul;34(8):1885-903.
45. Osuji IJ, Vera-Bolanos E, Carmody TJ, Brown ES. Pregnenolone for cognition and mood in dual diagnosis patients. Psychiatry Res. 2010 Jul 30;178(2):309-12.
46. Ritsner MS. Pregnenolone, dehydroepiandrosterone, and schizophrenia: alterations and clinical trials. CNS Neurosci Ther. 2010 Spring;16(1):32-44.
47. Ritsner MS, Gibel A, Shleifer T, et al. Pregnenolone and dehydroepiandrosterone as an adjunctive treatment in schizophrenia and schizoaffective disorder: an 8-week, double-blind, randomized, controlled, 2-center, parallel-group trial. J Clin Psychiatry. 2010 Oct;71(10):1351-62.
48. Khalsa DS. Integrated medicine and the prevention and reversal of memory loss. Altern Ther Health Med. 1998 Nov;4(6):38-43.
49. Vallee M, Mayo W, Le Moal M. Role of pregnenolone, dehydroepiandrosterone and their sulfate esters on learning and memory in cognitive aging. Brain Res Brain Res Rev. 2001 Nov;37(1-3):301-12.
50. Akan P, Kizildag S, Ormen M, Genc S, Oktem MA, Fadiloglu M. Pregnenolone protects the PC-12 cell line against amyloid beta peptide toxicity but its sulfate ester does not. Chem Biol Interact. 2009 Jan 15;177(1):65-70.
51. Meieran SE, Reus VI, Webster R, Shafton R, Wolkowitz OM. Chronic pregnenolone effects in normal humans: attenuation of benzodiazepine-induced sedation. Psychoneuroendocrinology. 2004 May;29(4):486-500.
52. Oberbeck R, Kobbe P. Dehydroepiandrosterone (DHEA): a steroid with multiple effects. Is there any possible option in the treatment of critical illness? Curr Med Chem. 2010;17(11):1039-47.
Written: By Julie Trevano
Article Source: http://www.lifeextension.com/Magazine/2011/7/State-of-California-Decrees-Strong-Warning-Labels-on-DHEA-and-Pregnenolone/Page-01
“The Greatest Health of Your Life”℠
Boston Testosterone Partners
National Testosterone Restoration for Men
Wellness & Preventative Medicinehttp://www.BostonTestosterone.com
http://www.facebook.com/bostontestosterone
855-617-MEDS (6337) -
Testosterone Deficiency in Men
It is not normal to wake up feeling tired all of the time, nor is it written in stone that the body has to break down as you age. Do not let any person or doctor tell you that lack of energy, weight gain, decreased sex drive, and loss of muscle are a fact of life. They are not! Why is it that some people manage to stay looking young and fit throughout their lives when others show the signs of aging in their early years? Testosterone deficiency may be to blame.
If the only thing you have ever thought testosterone was good for was building muscles, or increasing a man’s love drive, you are very mistaken. These are only two of the many functions testosterone has in the body. While often referred to as the male sex hormone, testosterone is beneficial to everyone, male and female, alike.Yes, you are getting older – we all are! That does not mean that you have to hang up your running shoes, put away your golf clubs, or cancel your gym membership. Once you understand the signs and symptoms of testosterone deficiency in men, you will be able to determine if the time has come to reach out to a specialist for help.
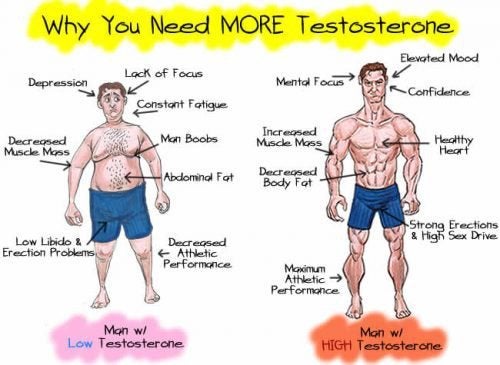
Here are the top warning signs that you might have testosterone deficiency:
- You are always tired – in the morning when you wake up, in the afternoon after eating lunch, at night after work
- You have gained weight – unless you have changed your eating habits and are now consuming mass quantities of food or alcohol beverages, abdominal weight gain is often a sign of hormonal imbalance
- Your sex drive is missing from action – there is no action here when your libido has disappeared, and you find it takes a long time to feel even the slightest bit aroused
- You can no longer achieve or maintain a powerful erection – erectile dysfunction is an immediate sign that something is wrong, and this can be as simple as fewer morning erections all the way to not being able to achieve an erection or orgasm
- You are shrinking – loss of height has everything to do with decreased bone density – a serious issue when Low T is present
- Your muscle size has decreased – testosterone helps to maintain muscle structure and strength, and if your workouts are no longer producing the desired effect, testosterone deficiency could be the problem
- You are feeling depressed – depression, mood changes, anxiety, aggression, lack of motivation, decreased drive, frustration – these are all signs of testosterone deficiency
- You forget things – memory failure, trouble with mental calculations, difficulty learning new things or committing new facts to memory, and poor focus are all associated with Low T
- Hair loss – balding or thinning hair on the head, and excess hair growth on the body may all signal low testosterone
- You have other health problems – if you have any of the following conditions you may also have testosterone deficiency: heart disease, diabetes, obesity, thyroid issues, osteoporosis, sleep apnea, Alzheimer’s disease, dementia, high blood pressure, osteoarthritis, or prostate problems
It is also not uncommon for a man with Low T to experience hot flashes and night sweats much the same way as a woman dealing with menopause. In fact, the term applied to Low T is andropause. The good news is that there is a way to improve these symptoms, you just need to know where to look and who to turn to for help.
Which Doctor Will Help to Reveal Testosterone Deficiency
The right doctor will help you determine if your symptoms are associated withtestosterone deficiency. Blood testing will reveal if testosterone or any other hormone levels are below their normal range. Some of these hormones impact one another, causing a spiraling effect of deficiencies. The doctor that you want to contact at this time is a hormone replacement therapy specialist – HRT for short. These practitioners work with men and women over the age of thirty who are experiencing changes in their bodies due to hormonal imbalances.
An HRT specialist will not brush off your symptoms as signs of aging. These doctors know that testosterone deficiency can create havoc in the body, and lead to serious illness if not caught and treated. A proper diagnosis will provide patient-targeted treatment that will bring stellar results.
You do not need to live with the symptoms outlined above. There is help, and a hormone replacement specialist can provide what you need to feel like yourself again. Vitality, libido, passion, and excitement can and should be a part of your life. Testosterone therapy can make it happen.
Article Source: http://positivemed.com/2016/06/21/testosterone-deficiency/
“The Greatest Health of Your Life”℠
Boston Testosterone Partners
National Testosterone Restoration for Men
Wellness & Preventative Medicinehttp://www.BostonTestosterone.com
http://www.facebook.com/bostontestosterone
855-617-MEDS (6337) -
Older men with higher testosterone levels lose less muscle mass as they age
A recent study accepted for publication in The Endocrine Society’s Journal of Clinical Endocrinology & Metabolism (JCEM) found that higher levels of testosterone were associated with reduced loss of lean muscle mass in older men, especially in those who were losing weight. In these men, higher testosterone levels were also associated with less loss of lower body strength.
Loss of muscle mass and strength contribute to frailty and are associated with falls, mobility limitations and fractures. Men lose more muscle mass and strength than women as they age, suggesting that sex steroids, and testosterone in particular, may contribute to body composition and physical function changes. This study sought to better understand the relationship between testosterone levels and healthy aging in older men and found that higher testosterone levels may help older men preserve muscle mass and delay frailty as they age.
“Our study finds that men, aged 65 years and older, with higher testosterone levels lost less muscle mass, especially in their arms and legs, than men this age who had lower testosterone levels,” said Erin LeBlanc, MD, of Kaiser Permanente Northwest in Portland, OR and lead author of the study. “Men who had higher testosterone levels before they lost weight also lost less leg function and could stand up more easily from a chair than men who had lower testosterone levels before they lost weight.”
In this study, researchers used data from 1,183 men aged 65 years or older and tested the hypothesis that higher baseline measures of sex steroids are associated with lesser declines in lean mass and maintenance of physical performance over an average follow-up of 4.5 years. Body composition was measured using dual energy x-ray absorptiometry (DXA) scans and physical performance was measured through a series of exercises that assessed grip strength, lower extremity power, walking speed and the ability to rise from a chair without the use of arms.
“The amount of testosterone men have in their bodies may contribute to how much muscle and strength they lose as they get older,” said LeBlanc. “Our study adds evidence to the growing body of literature that suggest higher levels of endogenous testosterone may be favorably associated with some key components of healthy aging in men.”
Other researchers working on the study include: Patty Wang, Christine Lee, Lynn Marshall and Eric Orwoll of Oregon Health & Science University in Portland; Elizabeth Barrett-Connor and Gail Laughlin of the University of California, San Diego in La Jolla, CA; Jane Cauley of the University of Pittsburgh in PA; and Andrew Hoffman of Stanford University in CA.
The article, “Higher testosterone levels are associated with less loss of lean body mass in older men,” appears in the December 2011 issue of JCEM.
Article Source: http://www.stonehearthnewsletters.com/older-men-with-higher-testosterone-levels-lose-less-muscle-mass-as-they-age/elder-care/
“The Greatest Health of Your Life”℠
Boston Testosterone Partners
National Testosterone Restoration for Men
Wellness & Preventative Medicinehttp://www.BostonTestosterone.com
http://www.facebook.com/bostontestosterone
855-617-MEDS (6337)
